Strabismus, also known “crossed eyes,” is a condition in which the eyes do not properly align with each other when looking at an object. It is mostly a visual disorder found in children with significant implications if not diagnosed and managed early.
Causes of Strabismus
Strabismus can be either congenital (present at birth) or acquired (develops later in life). Factors that contribute to the development of strabismus in children includes:
- Genetic Factors: A family history of strabismus increases the likelihood of a child developing the condition. Certain genetic syndromes, such as Down syndrome and cerebral palsy, are also associated with a higher incidence of strabismus.
- Neurological Disorders: Conditions that affect the brain, such as hydrocephalus or brain tumors, can disrupt the neural pathways controlling eye muscles, leading to strabismus.
- Refractive Errors: Significant differences in the refractive errors between the two eyes (anisometropia) can cause the brain to favor one eye, leading to strabismus. Hyperopia (farsightedness) is a common refractive error linked with the condition.
- Muscle Abnormalities: Problems with the extraocular muscles or the nerves that control these muscles can lead to misalignment of the eyes. For example, congenital cranial dysinnervation disorders (CCDDs) can affect the normal innervation of eye muscles.
- Injury or Trauma: Head injuries can damage the areas of the brain responsible for eye movement or the eye muscles themselves, resulting in strabismus.
Symptoms of Strabismus
The common symptoms of strabismus include:
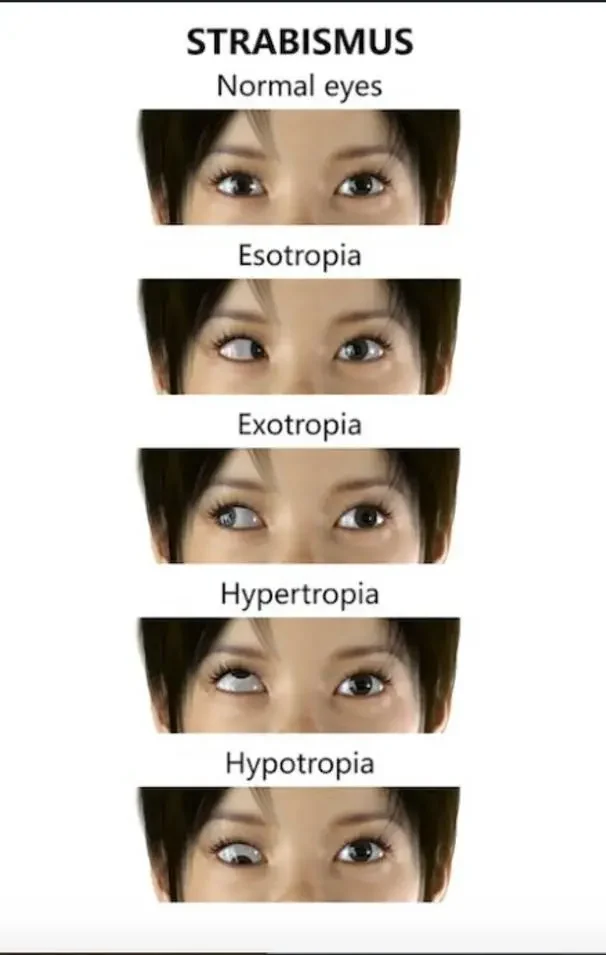
- Misaligned Eyes: One or both eyes may turn inward (esotropia), outward (exotropia), upward (hypertropia), or downward (hypotropia).
- Double Vision: Children might experience diplopia, or double vision, because each eye is sending a different image to the brain.
- Squinting or Closing One Eye: To avoid double vision, a child may squint or close one eye, especially in bright light or when tired.
- Head Tilting: Children may tilt their head to try to align their eyes and reduce double vision or to enhance their field of view.
- Poor Depth Perception: Difficulty in judging distances accurately can be a sign of strabismus, as proper depth perception relies on good binocular vision.
Management of Strabismus in Children
The management is aimed at achieving proper eye alignment and binocularity, improve visual acuity, and prevent amblyopia (lazy eye). The severity of the crossed eye determines the treatment. In addition, the child’s age and the underlying cause must be considered. The following are the primary management strategies:
1. Corrective Lenses
Glasses or Contact Lenses: Refractive errors, especially hyperopia, can cause or exacerbate the condition.
2. Occlusion Therapy
A patch may be placed over the stronger eye to encourage the use of the weaker eye. This can help improve visual acuity and reduce the risk of amblyopia. The use of Atropine eye drops to blur the vision in the stronger eye while encouraging the use of the weaker eye might help similar to patching.
3. Vision Therapy or Orthoptics
Involves a series of exercises designed to improve eye coordination and strengthen the eye muscles. These exercises must be supervised by an Optometrist/ Orthoptist. It majorly effective in cases of intermittent or mild strabismus.
**Use of prism lenses which are incorporated into glasses to bend light entering the eye, helps to reduce the eye’s turning and improve binocular vision.
4. Strabismus Surgery:
Blot is an invasive procedure so it’s only considered when other treatments fail correct the misalignment. The surgery involves adjusting the length or position of the eye muscles to align the eyes properly. This is typically an outpatient procedure, and children often recover quickly.
5. Monitoring and Follow-Up
Regular Check-Ups: Continuous monitoring by an eye specialist is crucial to ensure the treatment’s effectiveness and to make any necessary adjustments. Early and regular follow-up can prevent recurrence and address any new issues promptly.
6. Addressing Underlying Conditions
Treating Associated Medical Conditions: If strabismus is secondary to an underlying condition such as a neurological disorder, treating the primary condition is essential. Coordinated care with neurologists or other specialists may be required.
Conclusion
Early diagnosis and intervention are key in the management of strabismus to prevent long-term visual impairment. A child’s first eye examination should be at six months. With timely and appropriate treatment, many children with strabismus can achieve good visual outcomes and lead a normal life.